CHRONIC CERVICAL MYOFASCIAL SYNDROME
BACKGROUND
Pain attributed to muscle and its surrounding fascia is termed myofascial pain, with cervical myofascial pain thought to occur following either overuse or trauma to the muscles that support the shoulders and neck. In the cervical spine, the muscles most often implicated in myofascial pain are the trapezius, levator scapulae, rhomboids, supraspinatus, and infraspinatus. Myofascial pain in any location is characterized on examination by the presence of trigger points located in skeletal muscle. A trigger point is defined as a hyperirritable area located in a palpable, taut band of muscle fibers. The primary concern for patients with cervical myofascial pain is chronicity. Recurrence of myofascial pain is a common scenario. Prompt treatment prevents other muscles in the functional unit from compensating and, consequently, producing a more widespread and chronic problem. Migraine headaches and muscle contraction headaches are known to occur frequently in the patient with myofascial pain.Temporomandibular joint (TMJ) syndrome also may be myofascial in origin
ETIOLOGY
Cervical myofascial pain is thought to occur following either overuse or trauma to the muscles that support the shoulders and neck. Common scenarios among patients are recent involvement in a motor vehicle accident or performance of repetitive upper extremity activities. In the cervical spine, the muscles most often implicated in myofascial pain are the trapezius, levator scapulae, rhomboids, supraspinatus, and infraspinatus. Trapezial myofascial pain commonly occurs when a person with a desk job does not have appropriate armrests or must type on a keyboard that is too high.
EPIDEMIOLOGY
Occurrence in the India Myofascial pain is thought to occur commonly in the general population. As many as 21% of patients seen in general orthopedic clinics have myofascial pain. Of patients seen at specialty pain management centers, 85-93% have a myofascial pain component to their condition. Sex- and age-related demographics Cervical myofascial pain occurs in both sexes, but with a predominance among women. Myofascial pain seems to occur more frequently with increasing age until midlife. The incidence declines gradually after middle age.
PATHOPHYSIOLOGY
- Trigger points are known to elicit local pain and/or referred pain in a specific, recognizable distribution
- Palpation in a rapid fashion (ie, snapping palpation) may elicit a local twitch response, a brisk contraction of the muscle fibers in or around the taut band; the local twitch response also can be elicited by rapid insertion of a needle into the trigger point
- Restricted ROM and increased sensitivity to stretch of muscle fibers in a taut band are noted frequently
- The muscle with a trigger point may be weak because of pain; usually, no atrophic change is observed
- Patients with trigger points may have associated localized autonomic phenomena (eg, vasoconstriction, pilomotor response, ptosis, hypersecretion) An active myofascial trigger point is a site marked by generation of spontaneous pain or pain in response to movement; in contrast, latent trigger points may not produce pain until they are compressed.
CLINICAL PRESENTATION
- Cervical spine range of motion (ROM) is often limited and painful
- The patient may describe a lumpiness or painful bump in the trapezius or cervical paraspinal muscles
- Massage is often helpful, as is superficial heat
- The patient's sleep may be interrupted because of pain
- The cervical rotation required for driving is difficult to achieve
- The patient may describe pain radiating into the upper extremities, accompanied by numbness and tingling, making discrimination from radiculopathy or peripheral nerve impingement difficult
- Dizziness or nausea may be a part of the symptomatology
- The patient experiences typical patterns of radiating pain referred from trigger points
PHYSICAL EXAMINATION
- Patients with cervical myofascial pain often present with poor posture; they exhibit rounded shoulders and protracted scapulae.
- Trigger points frequently are noted in the trapezius, supraspinatus, infraspinatus, rhomboids, and levator scapulae muscles.
- The palpable, taut band is noted in the skeletal muscle or surrounding fascia; a local twitch response often can be reproduced with palpation of the area.
- ROM of the cervical spine is limited, with pain reproduced in positions that stretch the affected muscle.
- While the patient may complain of weakness, normal strength in the upper extremities is noted on physical examination.
- Sensation typically is normal when tested formally; no long tract signs are observed on examination.
DIFFERENTIAL DIAGNOSIS
Rheumatoid Arthritis
- Upper extremities (metacarpophalangeal joints, wrists, elbows, shoulders)
- Lower extremities (ankles, feet, knees, hips)
FIBROMYALGIA MYOFASCIAL PAIN SYNDROME Similarities  Pain in muscles
Pain in muscles  Decreased ROM
Decreased ROM  Postural stresses Differences ✗ Tender points ✗ Poor sleep ✗ No referred patterns of pain ✗ Fatigue ✗ Trigger points on muscles ✗ Referred patterns of pain ✗ Tight band of muscle .
Postural stresses Differences ✗ Tender points ✗ Poor sleep ✗ No referred patterns of pain ✗ Fatigue ✗ Trigger points on muscles ✗ Referred patterns of pain ✗ Tight band of muscle .
 Pain in muscles
Pain in muscles  Decreased ROM
Decreased ROM  Postural stresses Differences ✗ Tender points ✗ Poor sleep ✗ No referred patterns of pain ✗ Fatigue ✗ Trigger points on muscles ✗ Referred patterns of pain ✗ Tight band of muscle .
Postural stresses Differences ✗ Tender points ✗ Poor sleep ✗ No referred patterns of pain ✗ Fatigue ✗ Trigger points on muscles ✗ Referred patterns of pain ✗ Tight band of muscle . MEDICAL AND PHARMACOLOGICAL MANAGEMENT
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Tricyclic antidepressants
- Muscle Relaxants
- Nonnarcotic analgesics
- Anticonvulsants Medication
PHYSICAL THERAPY MANAGEMENT
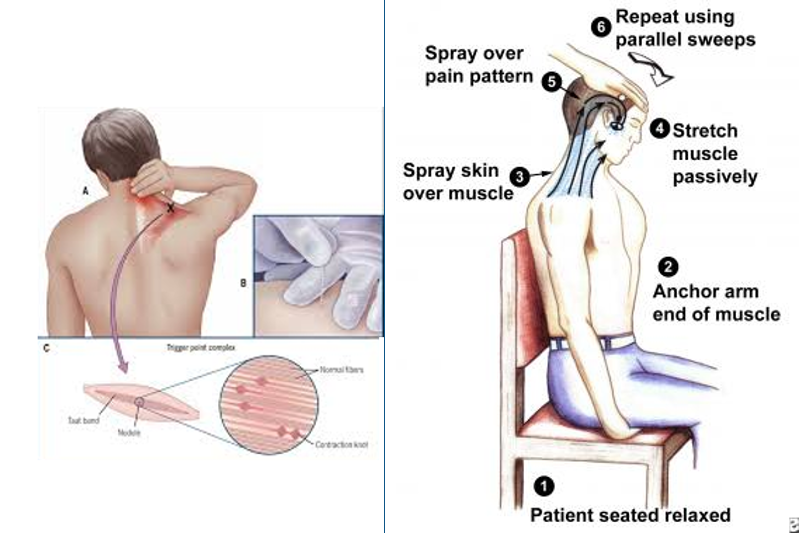
The primary goal of physical therapy is to restore balance between muscles working as a functional unit. The physical therapist may progress toward that goal initially by attempting to diminish pain. This goal can be accomplished using a modality-based approach performed in conjunction with myofascial release techniques and massage. Cervical stretch and stabilization are integral parts of the approach as well. Postural retraining is crucial in cervical myofascial pain. An ergonomic evaluation may be indicated if overuse in the work setting is contributing to the patient’s symptoms. Treatment consists of three main components: eliminating the trigger point, correcting the contributing factors, and strengthening the muscle. If the cause of the trigger point is a chronic overload of the muscle, the contributing factor should be eliminated prior to addressing the trigger point. When ROM is restored and the trigger point has been addressed, muscle strengthening is initiated. Several techniques are used to eliminate trigger points.
➔ Contract-relax-passive stretch done repeatedly until the muscle lengthens. ➔ Contract-relax-active stretch also done in repetition ➔ Trigger point release ➔ Spray and stretch ➔ Dry needling or injection.
References:
1.Kisner C, Colby L. Therapeutic Exercise. 5th Ed. F.A . Davis Company. 2007: 316-318 2.Travell JG, Simons DG. Myofascial Pain and Dysfunction. vol 2. Baltimore, Md: Lippincott Williams & Wilkins; 1992. 3.Hong CZ, Simons DG. Pathophysiologic and electrophysiologic mechanisms of myofascial trigger points.Arch Phys Med Rehabil. Jul 1998;79(7):863-72. 4.[Best Evidence] Sherman KJ, Cherkin DC, Hawkes RJ, Miglioretti DL, Deyo RA. Randomized trial of therapeutic massage for chronic neck pain. Clin J Pain. Mar-Apr 2009;25(3):233-8. 5.Ma C, Szeto GP, Yan T, Wu S, Lin C, Li L. Comparing biofeedback with active exercise and passive treatment for the management of work-related neck and shoulder pain: a randomized controlled trial. Arch Phys Med Rehabil. Jun 2011;92(6):849-582.
EVIDENCE- BASED PRACTICE Title: Differential Diagnosis and Treatment in a Patient With Posterior Upper Thoracic Pain Author: Stacie J Fruth Abstract: Determining the source of a patient’s pain in the upper thoracic region can be difficult. Costovertebral (CV) and costotransverse (CT) joint hypomobility and active trigger points (TrPs) are possible sources of upper thoracic pain. This case report describes the clinical decision-making process for a patient with posterior upper thoracic pain. Case Description. The patient had a 4-month history of pain; limited cervical, trunk, and shoulder active range of motion; limited and painful mobility of the right CV/CT joints of ribs 3 through 6; and periscapular TrPs. Interventions included CV/CT joint mobilizations, TrP release, and flexibility and postural exercises. Phys Ther. 2006;86:254 –268.] Results: This patient was able to return to his normal daily and recreational activities after 7 physical therapy sessions over the course of 4 weeks. He actively participated in his care, reported adherence to his HEP, and did not miss or cancel any sessions. His pain rating at rest decreased from an average of 7.5/10 to 0–1/10, and his pain rating with UE activities decreased from 9/10 to 1–2/10. Upon re-examination, the patient demonstrated symmetrical, nonguarded sitting and standing postures. Cervical, trunk and UE AROM were normal and pain- free. There was no pain and full strength during MMT. The patient said he had no pain with accessory motion testing of the right CV and CT joints or the upper thoracic spine. All of the patient’s initial physical therapy goals were fully met. He reported a considerable decrease in daily pain, full ability to play with and care for his children, unrestricted participation in softball, and minimal to no difficulty sleeping. This patient also was seen informally several times following his discharge. Each time he reported normal function and no residual pain. The last time this individual was seen was 5 years following his discharge, and he again reported full, pain-free function. Recommendations: This case suggests that CV/CT mobilizations and active TrP release may have been beneficial in reducing pain and restoring function in this patient. The author suggested that based on her estimation of joint hypomobility, the presence of pain with mobility assessment, and the limited available literature, I hypothesized that the patient might benefit from joint mobilizations. One similar description is in the literature regarding a patient with CV and CT joint dysfunction at ribs 2, 3 and 5. However, local analgesic injections were a part of the interventions and, therefore, a direct comparison with this case could not be made. Several aspects of this case report highlight the need for further research. Compared with the literature available in the lumbar and cervical areas, information regarding pain and dysfunction in the thoracic area is limited. There is also a lack of research concerning the reliability of assessments of joint mobility, the reliability of detecting of TrPs, the efficacy of providing joint mobilizations, and the efficacy of TrP release. Because these are all common physical therapist examination or intervention techniques, additional research is important to provide patients with evidence-based examinations and interventions.
BY
DR.SINDHU.B (PT)
