ROLE OF PHYSIOTHERAPY IN SYNOVIAL PLICA SYNDROME OF KNEE MANAGEMENT
Dr Deepika,
Consultant Physiotherapist, Rajaji Nagar, Spectrum Physio Center
Consultant Physiotherapist, Rajaji Nagar, Spectrum Physio Center
What is synovial plica syndrome?
A synovial plica is a shelf-like membrane between the synovium of the patella and the tibiofemoral joint. Plicae essentially consist of mesenchymal tissue which is formed in the knee during the embryological phase of development. This tissue forms membranes, which divide the knee into 3 compartments (the medial and lateral tibiofemoral compartments and the suprapatellar bursa).
This tissue usually starts to involute (fold inward) at 8-12 weeks of foetal growth, and is eventually resorbed, leaving a single empty area between the distal femoral and proximal tibial epiphysis: a single knee cavity. Movement of the foetus in the uterus contributes to this resorption. Yet, in many individuals the mesenchymal tissue is not fully resorbed and consequently the cavitation of the knee joint remains incomplete. The result is that in these individuals plicae can be observed, which represent inward folds of the synovial membrane in the knee joint. Various degrees of separation of the cavities are seen in the human knee. It is estimated that plicae are present in about 50% of the population.
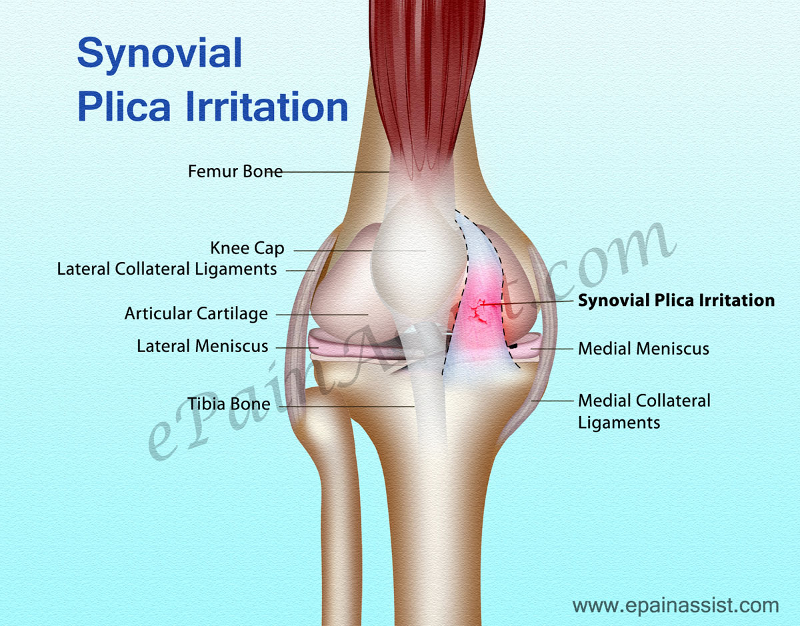
The elastic nature of synovial plicae allows normal movement of the bones of the tibiofemoral joint, without restriction. Yet, when repeating the same knee movement too often, such as bending and straightening the knee, or in the case of a trauma to the knee, these plicae can become irritated and inflamed. This can result in a disorder called the PLICA SYNDROME. It refers to an internal derangement of the knee which prevents normal functioning of the knee joint. It is particularly seen in children and adolescents and occurs when an otherwise normal structure in the knee becomes a source of knee pain due to injury or overuse.
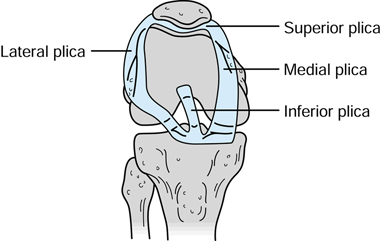
Types of Plica
In the knee, 4 types of plicae can be distinguished, depending on the anatomical location within the knee joint cavities: suprapatellar, mediopatellar, infrapatellar and lateral plicae. The plicae in the knee joint can vary in both structure and size; they can be fibrous or fatty, longitudinal or crescent-shaped
Etiology:
Synovial plicae mostly are asymptomatic and of little clinical consequences. This can be the result of various conditions, such as direct trauma or blow to the plica, blunt trauma, twisting injuries, repetitive flexion and extension of the knee, increased activity levels, weakness of the vastus medialis muscle, intra-articular bleeding, osteochondritis dissecans, torn meniscus, chronic or transient synovitis, When the initial injury has healed, patients can be symptom-free for some time, but then suddenly anterior knee pain can develop week or over months later. The term plica syndrome is used to refer to the internal derangement of the knee caused by an inflammation or injury to the suprapatellar, the medial patellar or the lateral plica, or a combination of the three, and which prevents normal functioning of the knee joint.
The medial plica is known to be the most commonly injured plica due to its anatomical location. The infrapatellar plica is normally not implied in the occurrence of the plica syndrome. The plica syndrome is thus often the result of excessive use of the knee and is therefore often encountered in people engaged in exercises involving repeated flexion-extension movements such as the ones seen in cycling, running, team sports, gymnastics, swimming and rowing sports and is particularly common in adolescent athletes.
CLINICAL PRESENTATION:
Plica syndrome can cause a series of symptoms, such as pain, clicking, popping, effusion, localised swelling, reduced range of motion, intermittent medial joint pain, instability and locking of the patello-femoral joint. It is more commonly seen in teenagers and young adults, even more so in women than in men.
Patients often report that symptoms are absent in the early phases of sporting activities but can come up suddenly and worsen progressively. They are often accompanied by a pain which can be described as intermittent, dull and aching and which will aggravate when performing patello-femoral loading activities such as walking up or down stairs, squatting, kneeling or after holding the knee in flexed position for some time.
When the symptoms occur, they are not easily distinguishable from other intra-articular conditions and knee derangements of the knee joint. The pain can be located at different places like the supra- patellar and the mid-patellar region when extending the knee. You can also hear cracking noises when flexing of extending the knee. The combination of contracting the quadriceps and the compression of the supra-patellar pouch can also be the cause of pain. What occurs frequently in patients with plica syndrome is that they often have a sense of instability when walking upstairs, downstairs or slopes.
PHYSICAL EXAMINATION
One of the most important points in diagnosing medial synovial plica pathology is obtaining an appropriate history from the patient. The pain is often described as a dull pain in the proximo-medial aspect of the knee and along the border of the patella. Frequently there’s is an internal hydrops and a string palpable. The pain increases with activity, overuse and is practically bothersome at night. Most patients have complaints when doing stairs, squats and standing up from a chair because these movements create a stress on the patello-femoral joint. The patient may also complain of pain following prolonged periods of sitting. About 50% of the patients let us know that they have been doing exercises with repetitive flexion and extension. Injury or overuse of the other plica can cause the same complaints, but these are seen less frequently.
SPECIAL TESTS:
Specific physical tests for the diagnosis of a medial plica include the plica and the mediopatellar plica stutter tests. Yet, the plica stutter test will not work when the joint is swollen. Other methods of examination that may indicate the presence of a medial plica include the medial subluxation test, McMurray’s, Appley’s test for instability and Cabot’s test.
MPP test is conducted with the patient in supine position and the knee extended. Manual force is then applied to the inferomedial part of the patellofemoral joint with the thumb, checking the presence of tenderness. If this tenderness clearly diminishes at 90° of flexion while applying the same manual force, the test is considered positive. When compared to arthroscopy, the sensitivity and specificity of this test were 89.5% and 88.7%, respectively, with a diagnostic accuracy of 89.0%.
Knee extension test or flexion test: For the active extension test, a quick extension of the tibia is performed as if making a kicking movement. The test is considered positive when painful, because of the abrupt tension on the plica from the quadriceps femoris muscle. The flexion test is performed by quickly swinging the tibia from a position of full extension into flexion and interrupting the swing between 30 and 60° of flexion. The test is again positive when painful, as the plica is then stretched with eccentric contraction of the quadriceps muscle.
The Plica Snap Test:
It can be used to verify if there is irritation of the medial plica. For the palpation of the medial synovial plica the patient lies supine on the examining table with both legs relaxed. For the medial synovial plica the examiner palpates the ligament by rolling the fingers over the plica fold, which is located between the medial border of the patella and the adductor tubercle region of the medial femoral condyle. Under the finger, which rolls directly against the underlying medial femoral condyle, the ligament will present itself as a ribbon-like fold of tissue. The test is positive when it reproduces the symptoms such as a sensation of mild pain. But also compare it with the normal knee to see if there is a difference in the amount of pain. It is demonstrated that it can be quite painful in some patients because the medial joint and synovium is well innervated.
MEDICAL MANAGEMENT
The treatment of a plica syndrome should initially be conservative in providing relief from symptoms by rest, using NSAIDs, physiotherapy, intra-plical or intra-articular corticosteroid injections. If non-operative measures fails, surgery should be considered.
Postoperative rehabilitation after plica resection usually goes quickly. Physical therapy is recommended starting 48 to 72 hours post-op, to prevent intra-articular scarring and stiffness. NSAIDs can be prescribed to reduce the risk of intra-articular fibrosis and to protect against plica recurrence. Most patients can resume sporting activities within 3 to 6 weeks. Yet, some variability in recovery time is possible and patients should make sure to allow full recovery before restarting physical activity or sporting.
PHYSIOTHERAPY MANAGEMENT
Conservative treatment of the synovial plica syndrome first consists of pain relief with repeated cryotherapy during the day using ice packs or ice massage, TENS, LASER, UST to reduce the initial inflammation. Other measures will include limiting aggravating activities by changing the daily physical movements to reduce repetitive flexion and extension movements and by correcting biomechanical abnormalities (tight hamstrings, weak quads).
Additionally, microwaves diathermy, phonophoresis, ultrasound and/or friction massage might be considered. Friction massage is also used in this therapy to break down scar tissue. Occasionally, immobilization of the knee in extended position for a few days can be helpful, as well as avoiding maintenance of the knee in flexed position during longer periods.
Once the acute inflammation is reduced, physical therapy can be initiated, aiming at decreasing compressive forces by stretching exercises and by increasing quadriceps strength and hamstring flexibility.
Treatment is usually recommended for the first 6-8 weeks after initial examination. It consists of strengthening and improving the flexibility of the muscles adjacent to the knee, such as the quadriceps, hamstrings, adductors, abductors, M Gastrocnemius and M Soleus.
The key components of the rehabilitation program will involve flexibility, cardiovascular condition training, strengthening and return to ADL. exercise to regain flexibility in extension is the supine passive knee extension exercise while placing a f
foam roller under the ankle. Gravity will help to stretch the knee in maximal extension. If possible you can make the exercise more difficult by putting weights on the anterior sight of the knee.
- Quadriceps sets
- Prone passive knee extension exercise, laying down on the belly, with knees over the bench (unsupported leg).
- Straight leg raises
- Leg presses
Also mini-squats, a walking program, the use of a recumbent or stationary bicycle, a swimming program, or possibly an elliptical machine are the most successful rehabilitation programs.
Rehabilitation programs will have the greatest success when focusing on strengthening the quadriceps muscles which are directly attached to the medial plica, and when avoiding activities which cause medial plica irritation.
The most important part of the quadriceps to train is the m. vastus medialis. Full range of quadriceps training is not recommended because these create excessive patellar compression at 90°. Instead straight leg raises and short-arc quadriceps exercises at 5°-10°, also hip adductor strengthening should be performed.
Other exercises to be performed are squad, go up and down the stairs and lunging forward. Other important components of this treatment are a stretching program for these muscles (quadriceps, hamstrings and gastrocnemius) and knee extension exercises.
The goal of these knee extension exercises is the strengthening of the tensor musculature of the joint capsule. But if the patient has too much pain when reaching terminal extension, then this should be avoided.
This conservative treatment is effective in most cases, but in some patients a surgery is necessary. In this case a post-operative therapy is necessary. The post-operative treatment is identical to the conservative treatment and is usually started 15 days after the surgery. The main goal of physiotherapy in plica syndrome is to reduce pain, maximize the ROM and increase the strength of the muscles.
The type of plica, the age of the patient and the duration of symptoms will greatly influence the success rate of conservative non-operative treatment of plica syndrome.
