- Regain full physical, psychological and social status
- Optimize long-term prognosis
- To promote and implement secondary prevention measures
Exercise training, education sessions, psychosocial support and support/counselling for patient and family in acute phase, out-patient care and long-term follow-up.
- Decrease cardiac morbidity and relieve symptoms
- Risk modification and secondary prevention
- Decrease anxiety and increase knowledge and self-confidence
- Increase fitness and ability to do normal activities
- Reassurance, support and information
- Behavioural change
- Exercise programme
PHASES OF CARDIO REHAB
Phase I - in-hospital (3-5 days)
Phase II - post discharge (2-6 weeks)
Phase III - outpatient programme (6-12 weeks)
Phase IV - long-term maintenance in community
- Increased cardiovascular endurance is the main aim
- Endurance training = activity using large muscle groups, can be sustained for a prolonged period and is rhythmic and aerobic resulting in an increase in maximal oxygen uptake.
- Maximal oxygen uptake (VO2 max) is limited centrally by cardiac output and peripherally by the capacity of muscles to extract oxygen from the blood.
- In healthy people = endurance training causes increase in CO as a result of increase in SV.
- Increased left ventricular mass and size
- Increased total blood volume
- Reduced peripheral resistance
Training-induced changes in muscles:
- Increased number and size of mitochondria
- Increased oxidative enzyme activity
- Increased capillarization
- Increased myoglobin
Factors that contribute to disease, can influence progression and future events
Exercise in healthy people cause:
- Raised metabolic rate
- Increased synthesis of HDL
- Improved insulin sensitivity
- Decreased blood pressure
Exercise reduces triggers in cardiac events:
- Prevents thrombus formation
- Improves endothelial function
- Reduces potential for serious arrhythmias
Borg 15-point scale or Borg CR10 scale
MET’s
Warm-up
Preparation for activity 15 minute
Low impact, dynamic movements of large muscle groups Take all major joints through normal ROM
Will delay onset of ischaemia by allowing enough time for coronary blood to flow in response to greater myocardial workload
Lessen risk of arrhythmias
Heart rate 20 bpm lower than lower end of prescribed training heart rate after warm-up ( 3 or 10-11 on Borg)
Aerobic exercises
Continious or interval approach
Interval approach – total volume of work done more, stimulus for physiological change greater
Circuit training – station 30s to 2 minutes
Individualisation – duration of station, intensity, period of rest and overall duration (increase duration before intensity)
By discharge patients should know signs and symptoms of excessive exertion and rate level of exertion
Home exercise programme for first 6 weeks, mostly walking Contact and telephonic follow-ups with rehabilitation services
FITT:
F + Time = 5-10 minutes, 2-3x daily and later 5-20 minutes, 1-2x daily
I = RPE < 11
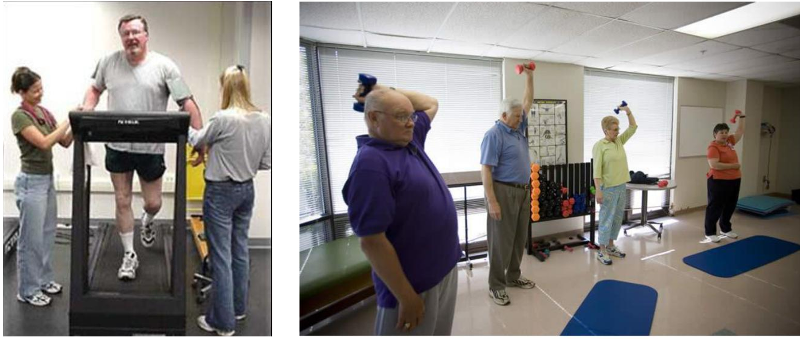
Programme implementation Outpatient exercise programme
Patient should be seen by physician or cardiologist before exercising
Patient safety during exercising very important Assessment of heart rate and blood pressure at rest and during exercising, RPE etc.
Risk factors for exercise
Patients should not exercise if not feeling well, symptomatic or unstable on arrival or with the
following:
- Fever, acute systemic illness
- Unresolved/unstable angina
- Blood pressure systolic > 200 mmHg and diastolic >110 mmHg
- Unexplained drop in blood pressure
- Symptomatic hypotension
- Tachycardia
- Arrhythmias
- Breathlessness, lethargy, palpitations, dizziness
- Unstable heart failure, weight gain > 2 kg in 2 days
- Unstable/uncontrolled diabetes
Programme management
All staff competent, appropriate skills and training, regularly updated
Appropriate emergency equipment, checked regularly, policy for handling emergency situations, appropriate venue
Patient education important - aims and exercise goals safety use of equipment
Programme management
Patients and families should know the following:
Signs and symptoms of exertion Importance of warm-up and cool-down Caution with isometric activities
Issue e.g. excessive heat/cold, dehydration
Avoid exercising after heavy meal, if ill an when tired Remain for 30 min after exercise for observation Excessive use of arm/upper body work results in higher systolic and diastolic blood pressure than the same work by legs
FITT-principles
1-2x per week rehabilitation class
2x per week home-based exercises walking the other days
aerobic exercises, 40-65% HRR or 60-75% HRmax
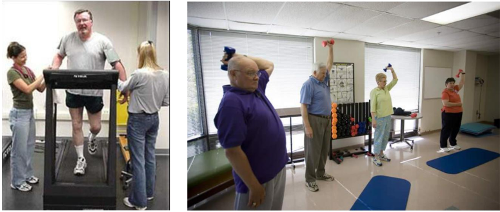
resistance training, 10-15 repetitions to moderate fatigue, 8-10 exercises, 2-3 times per week
FITT-principles
Aerobic, interval approach5-10 min, progress to 20-30 minutes warm-up 15-20 minutescool down > 10
Minutes.
Long-term community based exercise programme
Patient must be able to manage himself regarding exercises
Community-based instruct
Aerobic exercises
Exercise in lying not advised because:
Older patients have difficulty with transfers Increase in venous return – increases pre-load and myocardial load – increased risk of arrhythmias and angina
Orthostatic hypotensive episodes
Resistance training
Not previously used in cardiac patients:
increased blood pressure increased myocardial workload
Reduced ejection fraction and increased incidence in arrythmias, BUT also
increased diastolic pressure with better myocardial perfusion
10-15 repititions to moderate fatigue, 8-10 exercises
Cool down
10 minutes of movements of diminishing intensity and passive stretches of major muscles because:
increased risk of hypotension
In older patients heart rate takes longer to reach pre-exercise rates
raised sympathetic activity after exercise – arrhythmias